Leptospirosis: Recognizing the bacterial infection and preventing its spread.
Veterinary healthcare workers are at risk of exposure to infectious diseases that spread from animals to humans, also known as zoonoses. Possible sources of zoonotic infection include aerosolization, droplet spray, ingestion (oral), direct contact (animal, bodily fluids), indirect contact (e.g., fomite, contaminated tools and surfaces, or other objects in the environment), or vector-borne transmission of infectious agents from our patients.
General information.
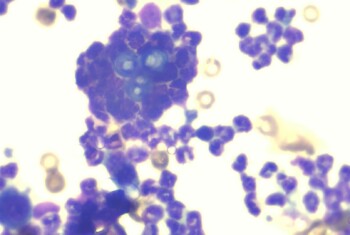
Leptospirosis is a zoonotic bacterial infection caused by various strains of a gram-negative spiral-shaped bacteria
called Leptospira. Dogs and rodents infected with Leptospira organisms can transmit infections to other animals and humans via direct or indirect contact with the bacteria. Commonly noted pathology in dogs includes nephritis/renal
failure, hepatic injury, and pulmonary hemorrhage.
How do people get leptospirosis?
- Exposure to the urine, body fluids, or tissues of infected animals.
- Asymptomatic animals can still shed organisms in urine!
- Infection generally enters through cuts and cracks in the skin or through the mucous membranes of the eyes, nose or mouth.
How would you know if you were infected?
Symptoms of leptospirosis can range from mild to severe. Clinical signs can develop anywhere from two days to four weeks after being exposed to the bacteria. Common symptoms of leptospirosis include:
- Fever
- Chills
- Headache
- Muscle aches
- Vomiting
- Diarrhea
- Abdominal pain
- Jaundice (yellowing of the skin and eyes)
- Skin rash
- Red eyes
To prevent spread.
- Appropriate cleaning solutions for disinfection include: 1:32 bleach, quaternary ammonium compounds,
 accelerated hydrogen peroxide solutions, and iodine-based disinfectants.
accelerated hydrogen peroxide solutions, and iodine-based disinfectants. - Any urine accidents should be cleaned immediately. Organic waste should be removed, followed by disinfection with appropriate cleaning solution and adequate contact time.
- Inactivate collected urine with disinfectant (ex. 1:1 aqueous dilution of 10% bleach for 10 minutes) before disposal. In patients with indwelling urinary catheters, disinfectant should be injected directly into the collection bag following catheter removal and prior to disposal.
- Blood, urine, and tissues from dogs suspected to have leptospirosis should be treated as medical waste and disposed of according to local regulations.
- All other waste materials (paper towels, etc.) should be double-bagged and brought to the dumpster immediately to prevent exposure to other pets or staff.
- High-pressure hoses should NOT be used to clean cages, floors, or runs, to reduce the risk of aerosolization of Leptospira organisms in urine. However, a hose can be used after the area has been properly disinfected.
- Laundry and bedding should be washed with detergent and bleach and dried thoroughly. Gloves, gowns, masks and face shields should be worn when handling soiled laundry.
- Kennel/cage should be disinfected once daily at a minimum.
- At discharge, after kennel has been cleaned and disinfected, kennel should also be steam cleaned according to appropriate guidelines if a steam cleaner is available.
Recommendations for safe patient handling.
- Patients with potential Leptospira infection should be housed in a floor-level, low-traffic area of the hospital where potential contact with their urine by other patients will be minimized.
- Patients’ cages should be marked with the appropriate infectious disease labeling system indicating he/she is a
 leptospirosis suspect.
leptospirosis suspect. - A tape border should be placed on the floor in front of the patient’s cage to limit foot traffic from hospital personnel or other patients.
- When transporting through the hospital, patients should travel via gurney to minimize environmental contamination with infected urine. Any urine leaks or points of contact occurring in transport should be cleaned/disinfected immediately.
- If urine cannot be contained, elimination areas cannot be effectively disinfected, or if the patient requires urine output monitoring, placement of an indwelling urinary catheter should be considered (instead of intermittent catheterization).
- Bathing and drying of hair that becomes soaked in urine is recommended.
- Patients being walked outside should be walked to a low-traffic area of the yard. Ideal area being a hard, non-permeable surface with access to direct sunlight. If the patient eliminates, the area should subsequently be disinfected with an appropriate disinfectant (see above).
- Laundry from the infected patient should be placed directly/immediately into a washing machine with detergent and bleach for routine laundering. If this is not possible, laundry should be placed in a labeled bag so that staff handling the laundry will be aware that barrier precautions (gloves/gown/mask/face shield) are needed for handling.
 accelerated hydrogen peroxide solutions, and iodine-based disinfectants.
accelerated hydrogen peroxide solutions, and iodine-based disinfectants. leptospirosis suspect.
leptospirosis suspect.