IBD: Diagnosis, types and treatment.
Inflammatory bowel disease (IBD) in dogs and cats is likely due to a variety of diseases that result in an accumulation of inflammatory cells within the lining of the stomach, small intestine, large intestine or a combination of these areas.
IBD upsets the dog digestive system to varying degrees and is usually classified according to the types of inflammatory cells present and the location affected. The causes of IBD are not well known, but are suspected to be a result of an abnormal response by the body to certain intestinal bacterial or dietary antigens (proteins).
Signs and symptoms of IBD.
The signs seen with IBD vary with the severity of the disease and the location affected.
Animals with IBD involving the small intestine usually present with:
- Chronic vomiting
- Weight loss
- Diarrhea
- Loss of appetite
- A combination of these problems
Animals with IBD involving the large intestine (chronic colitis) usually present with:
- Diarrhea with or without blood and mucous present
- Straining to defecate
- Increased urgency to defecate
- Occasionally vomiting
Diagnosis.
IBD can’t be diagnosed on physical examination, history, fecal checks, radiographs or laboratory work. These tests, however, are necessary to help rule out other diseases that may present with similar clinical signs, i.e., parasitic infections, intestinal foreign bodies, liver disease, kidney disease, metabolic diseases and cancer.
Blood studies are also helpful to assess metabolic status and screen for concurrent problems. Some dogs with severe IBD may have low protein levels in their blood due to loss of proteins through their intestines (protein-losing enteropathy). This finding may severely worsen the long-term prognosis for the patient.
Intestinal and stomach biopsies are ultimately necessary for a diagnosis. These can be obtained either endoscopically or surgically. The ultimate recommendation of endoscopic or surgical biopsies is made based on history, clinical signs, laboratory findings and diagnostic imaging studies.
The pathologist’s evaluation of biopsy samples will confirm the presence of IBD, specify the type of cellular infiltrate involved, stage the severity of the disease, and help to establish a treatment plan and prognosis for your pet.
Types of IBD.
Lymphoplasmacytic enteritis.
This is the most common form of IBD and is the result of an excessive accumulation of two types of white blood cells, lymphocytes 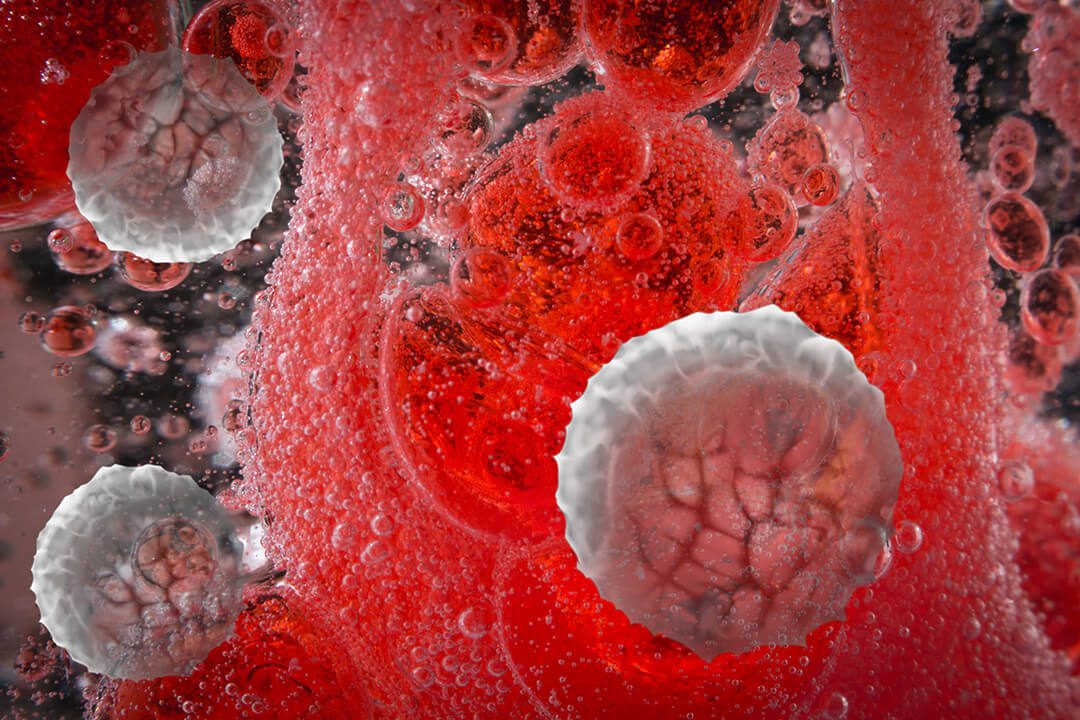 and plasma cells, in the lining of the gastrointestinal tract. Excessive protein loss from the bloodstream into the intestines is seen in very severe cases and is termed a protein-losing enteropathy.
and plasma cells, in the lining of the gastrointestinal tract. Excessive protein loss from the bloodstream into the intestines is seen in very severe cases and is termed a protein-losing enteropathy.
If inflammation is persistent and untreated, fibrosis (scar tissue) can result causing irreversible tissue damage. Lymphangiectasia (see below) may develop secondary to severe IBD. When lymphangiectasia is present, the prognosis is a great deal poorer as compared to those without this change.
Prognosis depends on the severity of the inflammation, presence of fibrosis, your pet’s body condition and response to therapy.
In cats, severe lymphocytic-plasmacytic enteritis may be a premalignant lesion, meaning that cancer (specifically lymphoma) may develop at a later date.
Eosinophilic enteritis.
This appears to be an allergic reaction to a dietary protein. A strict elimination diet in conjunction with medical therapy is often needed to resolve the signs. Prognosis is variable since some animals are unusually sensitive to many foods and are difficult to control.
Antibiotic-responsive diarrhea.
This occurs when there is an overgrowth of one or more bacterial species in the small intestine. The bacteria may be present because of anatomic defects, underlying intestinal disease, overuse of medications (frequently antibiotics) or for other unidentified reasons. The prognosis is often good.
Lymphangiectasia.
Though primary lymphangiectasia is not an inflammatory disease, the clinical signs may be much the same. This is an obstructive disorder involving the lymphatic system of the intestinal tract. The underlying cause is rarely found.
Secondary lymphangiectasia may develop in severe IBD. In either case, the prognosis is generally very poor. Small-to-medium breeds of dogs may initially respond fairly well to dietary and medical therapy, however, large breeds of dogs often do poorly despite dietary and medical therapy. Prognosis is often extremely poor.
Other.
Any disease that produces inflammation, infiltration, congestion or bleeding in the gastrointestinal tract can produce signs similar to IBD. Examples would include fungal disease, infiltrative cancers, advanced heart failure and chronic nonsteroidal or steroidal drug therapy. Low-grade intestinal lymphoma is commonly encountered in cats and rarely in dogs.
This is a slow-progressing disease with clinical signs that mimic those of inflammatory bowel disease. Unfortunately, surgical intestinal biopsies, rather than endoscopic biopsies, are typically required to confirm the diagnosis of intestinal lymphoma.
Treatment.

Dietary.
The goal of dietary management is to reduce the antigenic stimulation of the gastrointestinal tract’s immune system and to meet your pet’s nutritional requirements in an easily digestible form. This may be done with homemade diets (using recipes we provide you) or one of several commercially available diets.
Diet therapy is often critical in achieving control of these diseases. In some patients, a limited-ingredient diet with unique protein sources may be required.
Medications.
The goal of drug therapy is to “settle down” the immune response by suppressing the inflammation caused by the infiltration of cells into the gastrointestinal tract. Several types of anti-inflammatory drugs are used as the initial medications depending on the type of inflammation present. In patients with more severe disease, a combination of immunosuppressive medications may be prescribed.
- Corticosteroids (Prednisone, Prednisolone, Budesonide)
Prednisone and prednisolone are the primary anti-inflammatory drugs used because of their degree of effectiveness, as well as their low cost and wide availability.
Depending on the cause of the disease, most pets will show improvement in gastrointestinal signs within one to two weeks of starting appropriate therapy.
The primary side effects seen are dose related and include:
- Increases in
 thirst
thirst - Urination
- Appetite
- Anxiety
These can result in weight gain, agitation, restlessness and mood changes. These changes will resolve as the dose of the corticosteroid is reduced over the course of therapy.
Prednisolone is preferred in cats because many cats cannot adequately convert prednisone to prednisolone, the active anti-inflammatory ingredient.
Budesonide is a newer corticosteroid medication having largely local effects on the lining of the intestine with minimal absorption into the body. Budesonide may not be effective in dogs or cats with severe inflammatory bowel disease. Side effects are much less than those seen with other corticosteroid medications. Some patients, however, have side effects similar to those of prednisone or prednisolone. Budesonide is expensive, and the dosing of small pets requires recompounding of the medication.
- Metronidazole, Tetracycline, Doxycycline, Tylosin, Azithromycin
These are all antibiotics with or without weak anti-inflammatory effects.  These drugs may be used alone or in conjunction with other more potent anti-inflammatory drugs. These antibiotics may modulate or alter bacterial populations within the intestine, and may allow a lower dose of the other anti-inflammatory medications to be used. They may be used alone in animals suspected to have antibiotic-responsive diarrhea.
These drugs may be used alone or in conjunction with other more potent anti-inflammatory drugs. These antibiotics may modulate or alter bacterial populations within the intestine, and may allow a lower dose of the other anti-inflammatory medications to be used. They may be used alone in animals suspected to have antibiotic-responsive diarrhea.
- Cyclophosphamide (Cytoxan®)
Cytoxan® is used in pets that have serious side effects to the corticosteroids, are not fully responsive to corticosteroids, or require additional immunosuppressive medication because of the severity of disease. Side effects of Cytoxan® include bone marrow suppression (loss of ability to produce red and white blood cells and platelets) and sterile hemorrhagic cystitis (bloody urine). Because this is a potent drug, it is very important to monitor the CBC (complete blood count) in pets being treated with Cytoxan® on a regular basis (every four to six weeks). - Azathioprine (Imuran®)
This drug is also reserved for dogs that are not responsive to or having problems with corticosteroids. Although side effects are less than those with cyclophosphamide, this drug can also cause severe bone marrow suppression. As with cyclophosphamide therapy, there may be a recommendation that a CBC (complete blood count) be monitored on a regular basis (every four to six weeks). Azathioprine is very toxic in cats, so its use in cats is not recommended. - Chlorambucil (Leukeran®)
This drug is used in cats that either are not responsive to corticosteroids or as a sole anti-inflammatory drug in diabetic cats. Chlorambucil is generally used in conjunction with corticosteroids in cats with severe inflammatory bowel disease or those with low-grade small cell intestinal lymphoma. Although side effects are minimal, this drug can cause severe bone marrow suppression. As with cyclophosphamide therapy, there may be a recommendation that a CBC (complete blood count) be monitored on a regular basis (every four to weeks).
Results.
Some pets may require either long-term dietary management or low-dose medical therapy throughout their lives. Though IBD cannot be cured, the goal of treatment is to control the clinical signs without the need for medications. If any of the signs are seen, medical therapy may need to be re-instituted. Please contact your veterinarian before restarting any medication with your pet.
 thirst
thirst

