The Diagnostic Process for Gastrointestinal Diseases
Gastrointestinal signs (vomiting, diarrhea, regurgitation, weight loss, decreased appetite, abdominal distension and abdominal pain) are easily observed by clients and are often the reason for them bringing their pet to their veterinarian.
 However, the client’s interpretation of their pet’s clinical signs is sometimes misleading. A structured approach to the workup is essential in order to obtain a diagnosis and to provide the most expedient and effective treatment. Localizing the anatomic site of the disease (esophageal vs. stomach vs. small intestine vs. colon vs. systemic/metabolic) is also important to tailor the diagnostic plan. This article highlights some tips to streamline the diagnostic process and to avoid assumptions and pitfalls.
However, the client’s interpretation of their pet’s clinical signs is sometimes misleading. A structured approach to the workup is essential in order to obtain a diagnosis and to provide the most expedient and effective treatment. Localizing the anatomic site of the disease (esophageal vs. stomach vs. small intestine vs. colon vs. systemic/metabolic) is also important to tailor the diagnostic plan. This article highlights some tips to streamline the diagnostic process and to avoid assumptions and pitfalls.
History and Signalment
Obtaining a comprehensive and accurate history is one of the most important steps in the process of obtaining a diagnosis. Ask specific questions to distinguish among:
1. Dysphagia (oropharyngeal diseases): food is expelled from the mouth while trying to eat 2. Regurgitation (esophageal diseases): food is swallowed while eating but then expelled minutes to hours later and before being completely swallowed 3. Vomiting (diseases of the stomach/intestines or systemic/metabolic): active abdominal contraction; food is expelled after it has been fully swallowed
When possible, watch videos of the episodes or watch the pet eat.
Good Questions to Ask the Client
Regurgitation vs. Vomiting
1. When the pet expels food out, does it happen suddenly and surprise them so there’s no time for the client to put something on the floor to catch the material? (probably regurgitation). Typically no heaving sounds or movement prior to regurgitation and gagging sounds occur during or at the end of regurgitation.
2. Do the clients hear the vomiting happening with loud abdominal contractions minutes prior to their pet expelling the food out? (probably vomiting)
Timeline and Frequency
1. When did the vomiting (or diarrhea) start for this episode? When did the vomiting first start for any previous episodes? How many episodes have occurred and when have they occurred?
2. How often is the pet vomiting during each episode?
3. When was the last time the pet vomited?
4. Has the frequency of the vomiting changed?
5. Any change in diet? Any previous medications used to treat it? If so, how did their pet respond to the diet and/or medications?
6. Any other clinical problems (diarrhea, weight loss, decreased appetite, etc.) besides the problem that is the presenting complaint?
Weight loss with a good appetite
Weight loss with a poor appetite
Any combination of clinical signs can be present or not present.
Stool Consistency and Appearance
1. Purina Fecal Score (PFS): chart with pictures and description of stool; scale of 1-7; PFS 2 is perfect stool. Use to determine severity of diarrhea (chart is available online).
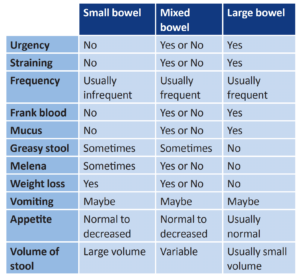
2. Large bowel diarrhea vs. small bowel diarrhea vs. mixed bowel diarrhea:
Age, Sex and Breed Can Provide Clues
Age
1. Young animals
- Gastrointestinal foreign material obstruction is a common cause of vomiting in young animals.

- Addison’s disease (hypoadrenocorticism) is more likely to occur in young animals.
- Infectious diseases such as parvovirus and/or GI parasitism are more common in young animals.
- Look for evidence of possible congenital abnormalities such as megaesophagus (especially if regurgitation is present).
2. Older animals
- Gastrointestinal cancer (lymphoma) is a common cause of vomiting in older animals (but it is possible at any age).
- Hyperthyroidism is a common cause of vomiting in older cats.
- Renal failure is a common cause of vomiting in older dogs or cats.
Sex
Female dogs are more likely to have Addison’s disease than male dogs.
Breed Predispositions
1. Large breed dogs
- Standard poodles: Addison’s disease
- German Shepherd dogs
– Megaesophagus +/- persistent right aortic arch (PRAA)
– Exocrine pancreatic insufficiency +/- inflammatory bowel disease
– Gastric dilatation-volvulus (GDV)
- Golden retrievers or Labrador retrievers
– Gastrointestinal or multicentric lymphoma
– Splenic or hepatic hemangiosarcoma
2. Small breed dogs
- Yorkies or Maltese
– Protein-losing enteropathy (PLE) +/- inflammatory bowel disease
– Portosystemic shunt (PSS)
- Miniature poodles: Addison’s disease
- Miniature schnauzers: Pancreatitis
Physical Examination Findings
Body Condition – in the Context of Appetite
1. Thin?
- Thin despite a good appetite: Major differentials include esophageal diseases (such as megaesophagus), primary gastrointestinal disease (inflammatory bowel disease versus gastrointestinal lymphoma versus severe gastrointestinal infection), exocrine pancreatic insufficiency (EPI), hyperthyroidism (cats), or diabetes mellitus.
- Thin with a poor appetite: Major differentials include primary gastrointestinal disease and chronic kidney disease.
2. Normal weight (or overweight)?
- Normal weight (or overweight) with a good appetite: Large intestinal diseases
- Normal weight (or overweight) with a poor appetite: Diseases outside of the gastrointestinal tract such as pancreatitis
Abdominal Palpation
1. Abdominal pain?
- Pancreatitis
- Gastrointestinal obstruction (obstructive mass; gastrointestinal FB, intussusception)
2. Abdominal distention?
- Enlarged stomach (gastric dilatation or gastric-dilatation volvulus)
- Enlarged abdominal organs
- Abdominal fluid (protein-losing enteropathy, pancreatitis)
3. Abdominal mass?
- Gastrointestinal origin
– Enlarged stomach
– Gastrointestinal foreign material obstruction
– Intussusception
– Gastrointestinal tumor
- Origin outside the gastrointestinal tract
– Enlarged pancreas
– Mass/tumor in an organ outside of the gastrointestinal tract
Extra-Abdominal Abnormalities
1. Oral exam – foreign material? Oral masses? Oral ulcers?
2. Throat exam – dilated esophagus? Thyroid slip?
3. Thoracic auscultation: Muffled lung sounds can be a sign of diaphragmatic hernia.
4. Peripheral lymphadenopathy? Dogs with gastrointestinal lymphoma can also have multicentric lymphoma. (However, normal peripheral lymph nodes do not rule out the possibility of gastrointestinal lymphoma.)
Laboratory
CBC/Chem/lytes, Urinalysis
1. Elevated kidney values along with unconcentrated urine can lead to a diagnosis of chronic kidney disease as the cause of the gastrointestinal signs.
2. Elevated liver values can be present in dogs with portosystemic shunt, liver failure, pancreatitis, and/or gallbladder disease.
3. Low sodium and high potassium +/- glucose can be a sign of Addison’s disease. Patient may have normal bloodwork and still have Addison’s disease. Dogs with atypical Addison’s disease can have normal Na/K and lack of a stress leukogram. Dogs with Addison’s disease typically have intermittent clinical signs.
4. Assess for concurrent problems that could affect treatment decisions
Fecal Flotation, Fecal Smear, Fecal PCR
1. Gastrointestinal parasites – can be a concurrent problem or can be the cause of the clinical signs; most of the gastrointestinal parasites are easy to diagnose
2. Giardia – can be hard to diagnose
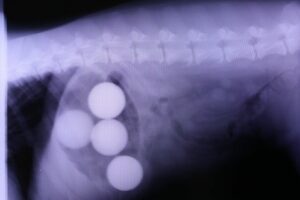
Imaging
Abdominal Radiographs
1. Assess serosal detail
2. Assess the shape, position, and relationship of the abdominal organs
3. Look for gastrointestinal foreign material and/or gastrointestinal obstruction. Gastric foreign material may be easier to diagnose with radiographs.
Abdominal Ultrasound
1. Check for abdominal fluid (abdominal ultrasound is sensitive for this).
2. Assess the thickness, motility, and layering of the gastrointestinal tract: Thickened intestines can be a sign of gastrointestinal inflammation (IBD), gastrointestinal neoplasia (lymphoma vs carcinoma vs other), or gastrointestinal infection (pythiosis) and location of the thickening can be helpful for planning follow-up diagnostics and plan (upper GI endoscopy vs. colonoscopy vs. both vs. exploratory laparotomy).
3. Look for gastrointestinal foreign material and/or gastrointestinal obstruction: Small intestinal foreign material and obstruction may be easier to diagnose with ultrasound.
4. Assess the extra-gastrointestinal organs for structure, nodules, or masses.
5. Assess the pancreas for signs of pancreatitis (ultrasound is more sensitive).
Chest Radiographs
1. Assess the esophagus
2. Check for concurrent aspiration pneumonia
Special Labs
GI Panel (B12/folate/TLI/PLI)
1. Low B12 +/- low folate are screening tests for primary gastrointestinal disease.
2. Elevated PLI is diagnostic for pancreatitis (but a normal PLI does not rule it out).
3. Low TLI is diagnostic for exocrine pancreatic insufficiency.
Baseline Cortisol
Screening test for Addison’s disease. If baseline cortisol > 2 ug/dL, this rules out Addison’s disease.
ACTH Stimulation Test
This is the definitive means to rule in or rule out Addison’s disease. If pre-ACTH and post-ACTH cortisol are <2 ug/dL, this is diagnostic for Addison’s disease. If they are > 2 ug/dL, Addison’s disease is ruled out.
Advanced Diagnostics
Upper Gastrointestinal Endoscopy +/- Colonscopy and Endoscopic GI Biopsies
1. Less invasive
2. The mucosal surface is visualized and assessed
3. Colonic tissue can be biopsied and colonic tissue samples can be submitted for tissue culture and fluorescence in situ hybridization (FISH) for diagnosis of granulomatous histiocytic colitis.
Exploratory Laparotomy and Gastrointestinal Biopsies
1. The gastrointestinal biopsies are full thickness and larger samples
More diagnostic samples
Only way to definitively rule out gastrointestinal cancer
2. Other organs can be assessed and biopsied at the same time.